Non-Radiographic Axial Spondyloarthritis
Reviewed by: HU Medical Review Board | Last reviewed: October 2022
Axial spondyloarthritis (axSpA) is a chronic disease in which the joints of the spine and the sacroiliac (SI) joints are inflamed. The SI joints connect the hips to the spine. This inflammation typically leads to pain in the hips, pelvis, and/or lower back.1
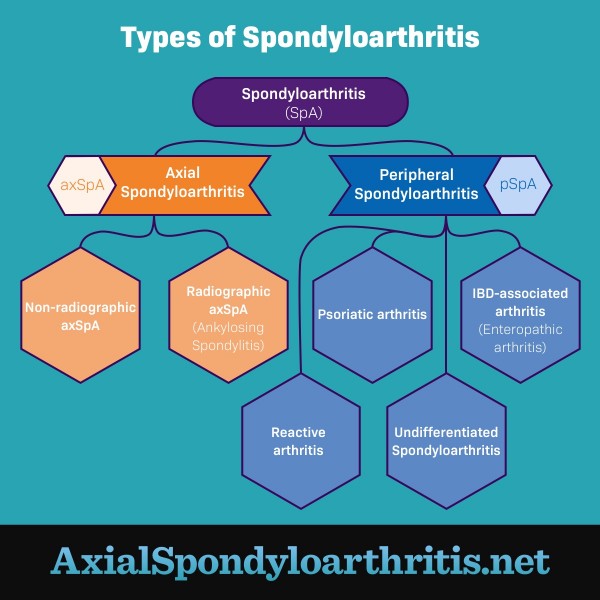
Figure 1. The different types of spondyloarthritis
What is non-radiographic axial spondyloarthritis?
There are 2 types of axial spondyloarthritis:1
- Non-radiographic axSpA (nr-axSpA) – Symptoms are present, but X-rays and MRI scans show little or no damage to the SI joints.
- Radiographic axSpA (r-axSpA) – Inflammation and damage to the spine and SI joints are visible on X-ray or MRI. Bones growing together at the joint (bony fusion) may occur. This condition is most commonly called ankylosing spondylitis (AS).
People with nr-axSpA often have the same symptoms as people with AS. But the 2 conditions exist on different parts of the axSpA disease spectrum. Some people with nr-axSpA may eventually begin to show joint changes on X-rays and progress to AS, but many will not.1,2
What are the symptoms?
The most common symptom of nr-axSpA is back pain. This pain is usually worse in the middle of the night or morning. Symptoms often begin in the teen years or young adulthood and almost always before age 45.2
Symptom severity is different for everyone. Severe pain, stiffness, and fusion of the spine or SI joints can occur. While nr-axSpA may cause mild pain and stiffness for years, it may never progress to spinal fusion.2
What causes non-radiographic axial spondyloarthritis?
This type of arthritis is caused by the body’s immune response (inflammation). Many other types of arthritis are caused by joint damage that results from overuse. That’s why people with nr-axSpA tend to feel better after exercise or stretching. People who have a slipped disc, on the other hand, feel better when they stay still.2
How is it diagnosed?
Because nr-axSpA and AS often have the same symptoms, doctors rely on recognizing patterns when making a diagnosis. They do this using a combination of exams and tests, including:3
- Physical exams
- Detailed family and medical history
- X-rays, which can be negative in both AS and nr-axSpA
- MRI, which shows inflammation of the SI joints in AS only
- Blood tests that look for genetic and inflammatory markers
Knowing how nr-axSpA and AS are similar and different helps doctors narrow down a diagnosis.1,3
Similarities between nr-axSpA and AS include:1-3
- They are diagnosed equally as often.
- Signs of the disease are similar in both conditions (primarily, back pain that lasts longer than 3 months).
- Both conditions can cause severe pain and disability. Also, both conditions can be mild with minimal symptoms.
Differences between nr-axSpA and AS include:1-3
- Studies show that axSpA may present differently in women than it does in men. Women are less likely to have damage that is visible on an X-ray, so they are more often diagnosed with nr-axSpA than with AS. But this does not mean that women have less severe symptoms or disease outcomes.
- The first place where a person feels pain also tends to differ between men and women. While men usually feel their first axSpA symptoms in their lower back, women are more likely to feel them in their neck or other joints.
- Elevated inflammatory markers in the blood are less common in people with nr-axSpA than in those with AS.
- A genetic marker called HLA-B27 is much more common in those with AS than those with nr-axSpA. But this marker also can be present with nr-axSpA. Many with HLA-B27 do not develop disease. Still others with AS or nr-axSpA do not have the marker.
Related conditions
Psoriatic arthritis (PsA) and arthritis with inflammatory bowel disease (IBD) commonly occur in people with nr-axSpA. This is because both PsA and arthritis with IBD fall under the spondyloarthritis umbrella.1
About 15 percent of people with nr-axSpA also get uveitis, a painful eye inflammation that causes redness and blurred vision.4
How is it treated?
The main goals of treatment for axial spondyloarthritis, including nr-axSpA, are to:5
- Decrease pain and stiffness
- Prevent joint and spinal deformities and fusion
- Maintain and improve daily function
Many people with axSpA find that medicines are essential to their treatment. Some of these medicines include:5
- Non-steroidal anti-inflammatories (NSAIDs) – These are the first-line drugs for treating axSpA. They include drugs like ibuprofen or naproxen.
- Pain relievers – Your doctor may suggest acetaminophen (Tylenol) to relieve some of your pain from axSpA. Stronger prescription pain relievers are not used as often because of their harmful side effects and risk of dependency.
- Biologics – These drugs are usually used to treat more severe disease or if you do not respond well to NSAIDs. The most common type of biologic used for axSpA blocks a protein called tumor necrosis factor (TNF). If an anti-TNF drug does not work, your doctor may prescribe a different type of biologic.
Talk to your doctor about which medicines might be right for you.
Regular exercise and daily movement are also important. Working with a physical therapist (PT) who is an expert in treating the spine is strongly advised. Your PT can help you develop a program that helps you maintain range of movement and relieve pain. Talk to your doctor about how you can find a PT in your area.5
While nr-axSpA has no cure, treatment and exercise can help. Knowing the facts and symptoms of nr-axSpA can help you better manage your disease. Remember, nr-axSpA does not always progress to spinal fusion and disability. Work with your doctor to ensure you get the treatment you need to manage the condition better.1-3