Radiographic Axial Spondyloarthritis (Ankylosing Spondylitis)
Reviewed by: HU Medical Review Board | Last reviewed: October 2022
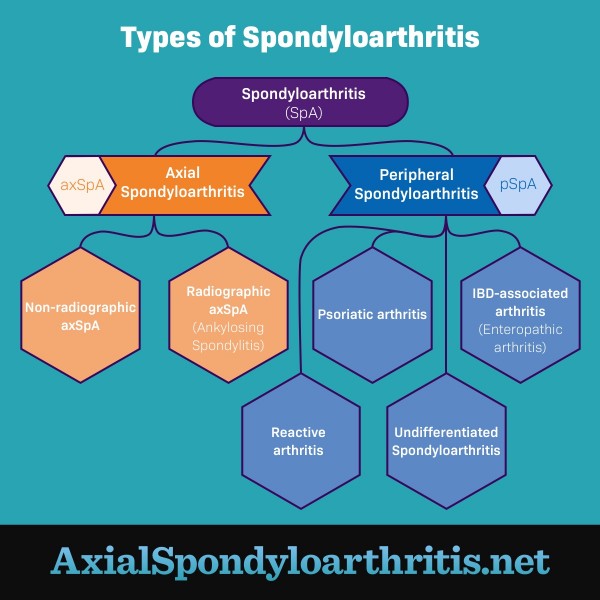
Axial spondyloarthritis (axSpA) is a general term used for 2 types of arthritis that affect the spine: radiographic axial spondyloarthritis (r-axSpA) and non-radiographic axial spondyloarthritis (nr-axSpA).1
What is ankylosing spondylitis?
Radiographic axial spondyloarthritis (r-axSpA) is commonly called ankylosing spondylitis (pronounced “ankle-oh-sing spohn-dih-lie-tiss"). It is a chronic inflammatory disease that affects the spine and sacroiliac (SI) joints. It is called radiographic because evidence of the condition can be seen on imaging tests such as X-ray and magnetic resonance imaging (MRI).1
Nr-axSpA, on the other hand, often has the same symptoms as ankylosing spondylitis (AS) but does not appear on imaging tests.1
Figure 1. The different types of spondyloarthritis
What are the symptoms?
AS, or r-axSpA, causes severe, chronic pain and stiffness in the affected joints, which are most often the spine and hips. People with AS typically have pain in their sacroiliac (SI) joints, where the hip bones (pelvic bones) meet the base of the spine. Some people also have pain and inflammation in other joints, such as:1,2
- Shoulders
- Ribs
- Hands
- Feet
The back and joint pain typically are worse after periods of rest and feel better after activity. AS can cause morning stiffness lasting longer than 30 minutes as well as buttock pain. As the condition progresses, it can cause joints in the spine to become fixed or fused. This can lead to loss of mobility and/or a curved posture.1
Who gets ankylosing spondylitis?
AxSpA usually begins between the ages of 20 and 30. But the condition can occur at any age. In the past, doctors thought AS was much more common in men. They now think that while men are diagnosed more often than women, the disease may not be any more common in men. Men just tend to have more spinal changes that show on X-ray than women do.3,4
AS occurs more frequently in white adults than Black adults. But Black adults tend to have more severe disease and greater levels of impairment. The exact number of people with nr-axSpA and AS is not known.5
What causes ankylosing spondylitis?
Doctors do not know the exact cause of AS. They think a combination of genes and environment leads to symptoms.1
Several genetic mutations have been linked to AS. The most common is the HLA-B27 genetic marker. But not everyone who has these genetic mutations will develop AS. Also, many people with AS do not have any of the genetic mutations known to be linked to the condition.1,4
How is it diagnosed?
Usually, a rheumatologist makes the diagnosis. Diagnosing AS involves a combination of tests and exams, including:1,4
- Physical exam
- Medical history
- Family history
- X-rays
- MRI scans
- Blood work
Does non-radiographic axSpA always progress to radiographic axSpA?
Nr-axSpA and r-axSpA (AS) are 2 conditions on the same spectrum. Both are considered axial spondyloarthritis. But nr-axSpA does not show up on X-rays, and AS does.1,3
This does not mean the pain is more severe in one or the other condition. Symptom severity can be the same across the disease spectrum. Some people who are originally diagnosed with nr-axSpA develop AS over time. Many others do not.1,3
How is it treated?
While there is currently no cure for AS, there are several ways to treat it. Treatment usually involves a combination of medicines, physical therapy, and exercise. In some severe cases, surgery may be recommended. Many people with AS also find at-home methods helpful in relieving symptoms, such as dietary changes or hot and cold packs.1,3