Digestive System and Axial Spondyloarthritis
Sometimes I feel like the number of ways AxSpA can affect my body are endless. It’s extremely discouraging. But as a systemic disease, the truth of the matter is that AxSpA can potentially disrupt the operations of most major organ systems in the body.
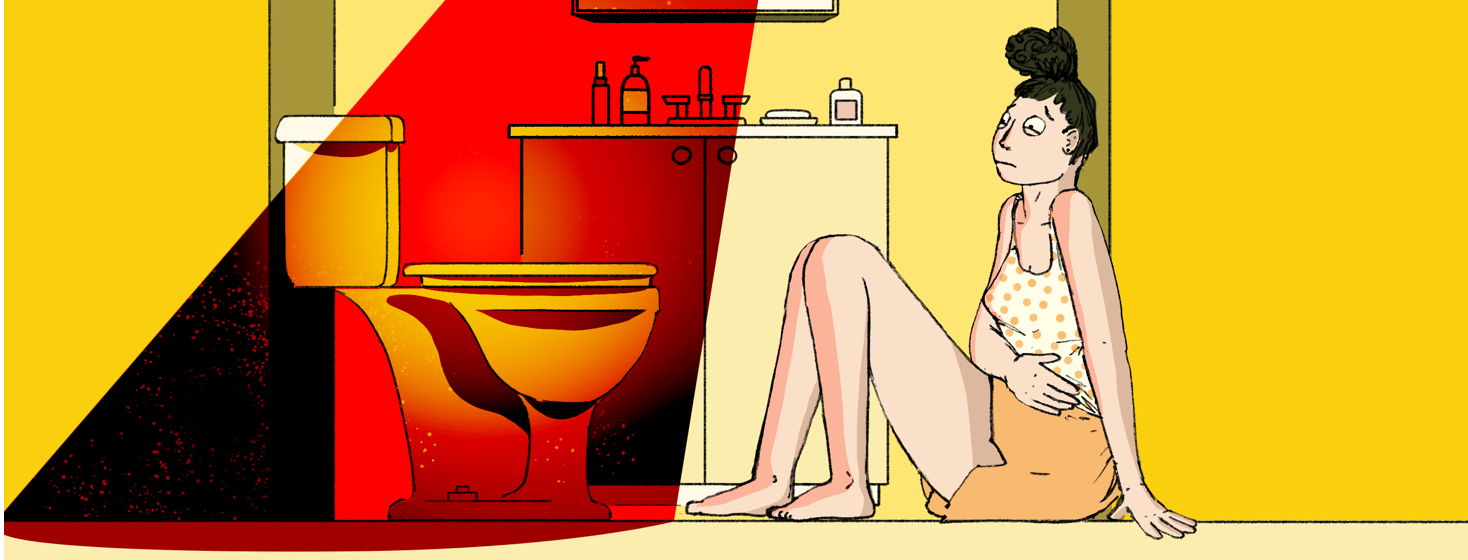
For the past year and a half, I’ve been managing some gastrointestinal issues that may or may not be directly related to my axial spondyloarthritis. The verdict is still out. But while I wait for results and answers (a wait that, if my decade and a half wait for my AS diagnosis is any indication, may last several more years), I thought I might explore what my experience has been like, what I know already, and what the research says.
My recent experience with GI discomfort and ankylosing spondylitis
It’s almost as unpleasant discussing gastrointestinal issues as it is living with them...almost! So I held off talking to my doctor about my stomach issues for nearly a year, hoping they would resolve on their own. When they didn’t resolve, I discussed the issues with my rheumatologist.
I’ve been dealing with periodic stomach pain and constant, daily bouts of loose stool that borders on diarrhea at times. At first, I thought these symptoms could be associated with my switch to methotrexate, to the point where I willfully believed that a change in medication would be a simple solution to some very frustrating symptoms.
My rheumatologist assured me that methotrexate could cause the GI symptoms I described, but since I was only taking my dose of methotrexate once a week, I should not be experiencing GI issues every other day of the week as well. So, she referred me to a gastrointestinal specialist.
Featured Forum
View all responsesVisiting the GI specialist
Since I have also been experiencing periodic swallowing difficulties, and since there’s a strong history of Crohn’s disease and ulcerative colitis on my mother’s side of the family, the GI specialist immediately decided to perform an upper and lower endoscopy.
While the immediate findings are in, I have not yet discussed the implications of these findings with my specialist. But I certainly didn’t leave there empty-handed, so to speak. During the endoscopies, the specialist recorded three stomach ulcers, some moderate GERD (which was no surprise to me), a mid-sized hiatal hernia, and severe stomach inflammation.
What’s still unclear at this point is the cause of the daily loose stool, along with the relationship of these symptoms to my AxSpA. Is it the axial spondyloarthritis that’s causing stomach inflammation? Or is there a relationship between my previously diagnosed AxSpA and some form of irritable bowel disease or syndrome?
The doctor did recommend avoiding NSAIDs for the foreseeable future, which is a recommendation I wish I didn’t have to follow. But since I had been self-medicating my back pain with ibuprofen for a decade before my diagnosis, I understand how that long-term NSAID use may have caused my stomach ulcers. At this point, it’s best not to cause more stomach damage, even though ibuprofen is the only OTC pain medication that helps with my joint pain.
Moreover, the specialist also told me that, since I’m already on Humira and methotrexate, two medications used to treat inflammatory bowel disease, if I did have IBD it was likely well controlled already. In other words, if IBD is the culprit, I’m already being treated for it.
For now, I wait for more information and do what research I can in the meantime. Hopefully, I’ll have more answers sooner than later.
What the research says
There are many studies on the prevalence of inflammatory bowel disease and irritable bowel syndrome in people with axial spondyloarthritis or ankylosing spondylitis. One such study indicates that 30.1% of patients with AS also have IBS.1 Another study notes the prevalence of IBD in people with AS “ranging from 6% - 14%.2
Clearly, the correlation here is not rare, and it’s not a one-way street either. In fact, another article indicates that “several studies have estimated the occurrence of spondyloarthropathies (SpA) in patients with IBD ranging between 17% and 39%, confirming that SpA is the most frequent extraintestinal manifestation in patients with IBD.”3
Whether I end up developing IBS and IBD is yet to be determined. I do understand that having one chronic disease often increases the likelihood of developing another. And while I don’t know anyone in my family with AS (or AxSpA), I do have multiple family members with IBD. That’s not enough to predict my future, I know, but it’s a strong indicator of what may be to come.
While I wait to hear more from the gastrointestinal specialist, I’d be interested in hearing if you also experience digestive system symptoms with your AxSpA. Does your AxSpA affect your GI health? Are you in the percentage of people with AxSpA and IBD?
Join the conversation