Gut Issues and Trying to Find Answers
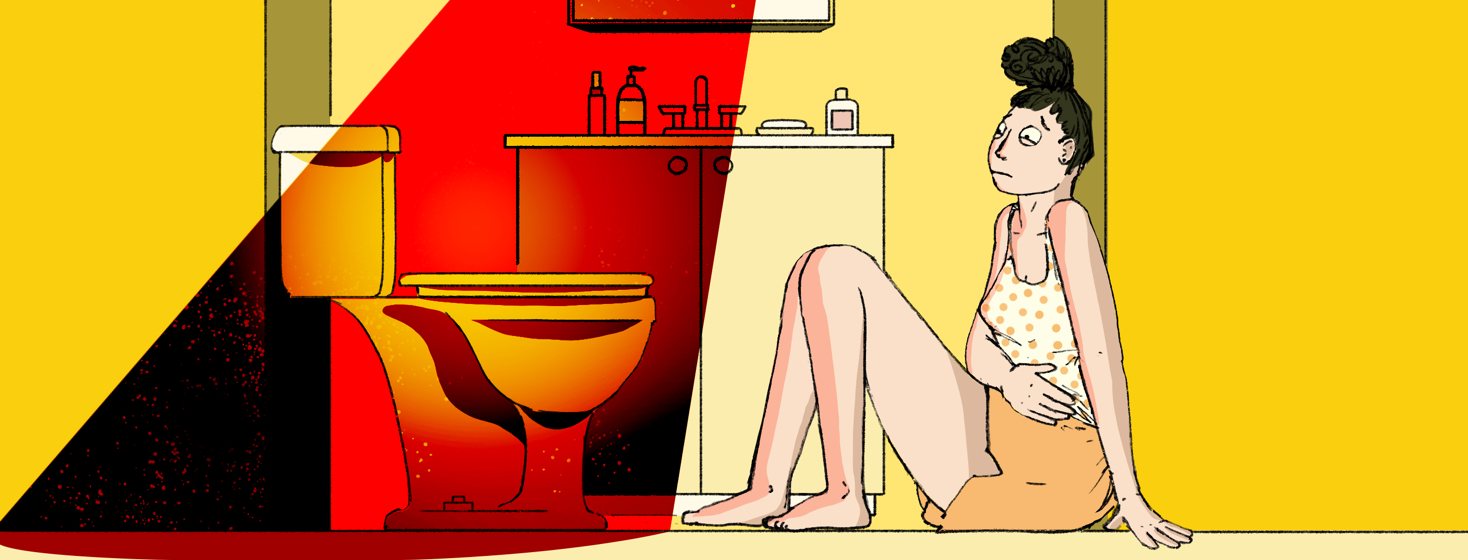
If I were told to choose one system that I didn’t want to malfunction and impede on my daily life, the digestive system would have definitely been in my top 3. But unfortunately for us all, this is real life, and we do not get to pick and choose which systems work like well-oiled machines and which ones will inevitably fail us and make us absolutely miserable.
Featured Forum
View all responsesI was forewarned this may happen
When I was initially diagnosed with AS, I was told by several different physicians that IBD often likes to “cohabitate” with AS. A small part of me was worried by this because for one, I suffered badly from IBS-C and lactose intolerance as a child. On top of that, I have an extensive family history of pretty much every type of digestive issue/disease on the planet including, but not limited to GERD, stomach ulcers, EOE, Crohn's disease, colon cancer, and ulcerative colitis.
Research
As usual, my curiosity got the best of me, and I headed straight to google. Through my research, I learned that sometimes AS can “foretell” the development of IBD, and the one that tends to show up is Crohn’s, but not always. Still, I didn’t exhibit any symptoms of IBD or any other type of digestive issue, so I pushed it to the back of my mind and went about life.
Bowel habits begin changing
In May of 2021 (close to two years from the onset of my AS), I had a stent placed in my left iliac vein. I’ve previously written about my experience with that procedure and how it sent me into one of the worst AS flares I’ve experienced thus far, but what I didn’t mention (or even catch on to at that point) was that it was also the beginning of a change in my bowel habits.
Constipation
Talking about one's bathroom habits is far from glamorous, but this is far more common in this community than people may realize, so I do feel it is important to be super transparent about my experience. With that being said, I did not have a bowel movement for 8 days after that procedure. Yes, 8. I was drinking Miralax daily and taking in as many fluids as I could and then finally broke into the magnesium citrate. On day 9, I was FINALLY able to have a BM! That is pretty much where the good news stops in my story though, and things only get crappier from here.
An unbreakable cycle
This cycle of chronic constipation wouldn’t end. I even asked my vein surgeon if they had ever seen anything like this after that procedure, and of course, the answer was no. Great. To make matters worse, in July I started experiencing pain in my upper abdominal area that made me extremely nauseous. I was taking Zofran like they were candies just to function. At a routine appointment with my rheumatologist, I asked her if it could in any way be connected to my AS because I was also flared up, but she, of course, said most likely not. She did, however, refer me to a gastroenterologist and just in time too, because around this time is when the really severe episodes that changed my thought process about all of this began.
Join the conversation