Vision Problems (Uveitis) and Axial Spondyloarthritis
Reviewed by: HU Medical Review Board | Last reviewed: January 2023 | Last updated: April 2024
Axial spondyloarthritis (axSpA) is an inflammatory form of arthritis. The chronic inflammation that comes with axSpA causes swelling and pain, mainly in the spine but also in other places in the body. Symptoms that you may feel outside of the spine or other joints are called extra-articular symptoms. One of these symptoms is inflammation in the eye called uveitis.1
This or That
Have you experienced uveitis?
What is uveitis?
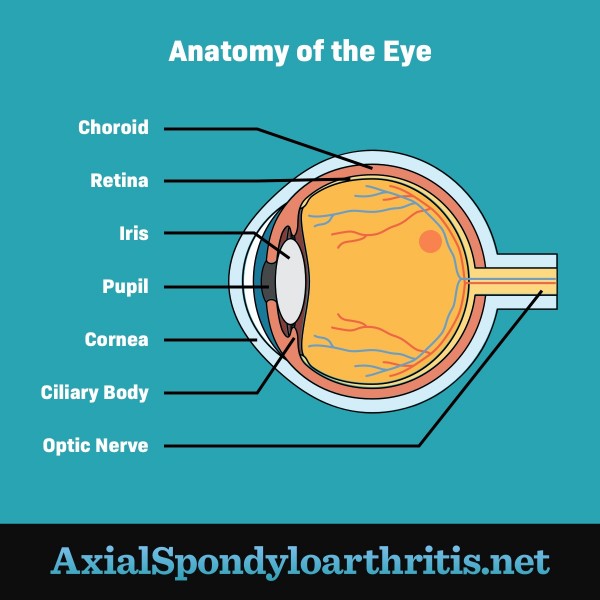
Uveitis is a painful condition that causes inflammation in the uvea. The uvea is the middle layer of the eye. It includes:2
- The iris – The colored part of the eye
- The ciliary body – A part that helps to focus light on the retina
- The choroid – A layer of blood vessels that provides oxygen and nutrients to the eye
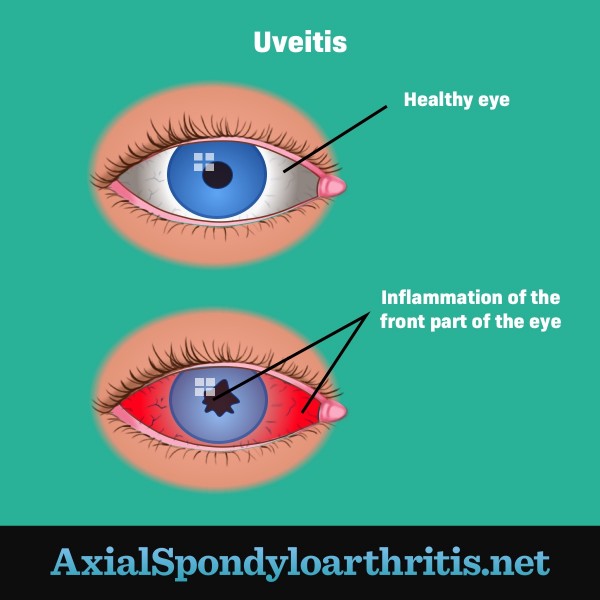
Uveitis can affect one or both eyes. It can occur at any age. The condition makes the eye red, cloudy, and sensitive to light. It can also lead to vision loss if left untreated.2
Up to 1 in 3 people with axSpA will get uveitis. In most cases, the condition is sudden, and treatment is effective. In rare cases, uveitis occurs often and is harder to treat.3
Figure 1. Anatomy of the eye
Symptoms of uveitis
Usually, uveitis symptoms appear suddenly and worsen quickly. Symptoms can include:2
- Eye pain
- Eye redness
- Cloudy or blurred vision
- Sensitivity to light
- Dark spots, or “floaters,” in the field of vision
- Increased tear production
Figure 2. The parts of the eye uveitis affects
Why does uveitis happen with axial spondyloarthritis?
Uveitis can result from injury, infection, or an autoimmune reaction. In an autoimmune reaction, the immune system mistakes healthy cells for foreign invaders and attacks them. Sometimes, the exact cause of uveitis is not known. But in people with axSpA, uveitis likely occurs because their immune system has triggered an inflammation response.2,3
How is it diagnosed?
When you see an eye doctor (ophthalmologist), they will do a full exam and ask questions about your health history. Some tests your doctor may perform include:4
- Vision tests – By having you read an eye chart, your doctor can check how well you can see.
- Eye pressure exam – This test measures the amount of pressure inside your eyes. This is known as tonometry. Your doctor will place numbing drops on your eyes to make the exam more comfortable.
- Pupil dilation – Here, your doctor places drops on your eyes to open up (dilate) your pupils. This allows your doctor to see the back of your eyes.
- Slit-lamp exam – In this test, your doctor shines a bright light in your eyes while using a microscope to examine the front and back of your eyes.
Your doctor might order other tests as well, including:4
- Blood tests
- Imaging tests, like a computed tomography (CT) or magnetic resonance imaging (MRI) scan
- Other advanced tests of the eye
How is it treated?
The goal of uveitis treatment is to decrease eye inflammation. Treatment can last several weeks or months, depending on the severity and cause of uveitis. Medicines used to treat uveitis include:4
- Steroids – Corticosteroids, or steroids, are potent anti-inflammatory drugs. Your doctor will likely first prescribe steroid eye drops to manage uveitis symptoms. If inflammation is behind the front of your eye, you may need a steroid shot or pills.
- Anti-spasm drugs – Uveitis can cause the muscles in the eye to tighten or spasm. This can lead to pain. Eye drops that control these spasms and widen your pupils might help with pain relief.
- Antibiotics – Your doctor will order antibiotic pills or drops if you have an infection.
- Drugs that affect your immune system – If both of your eyes have symptoms or your symptoms do not respond to other treatments, you may need to take an immunosuppressant drug. This type of drug works to turn down your immune system, which might help stop it from attacking the healthy cells in your eyes.
The time it takes to recover from uveitis depends on the type and severity of your symptoms. Uveitis that affects the back of your eye takes longer to heal than uveitis that affects the front of your eye. If you have severe inflammation, it will take longer to go away than if you have mild inflammation.4
It is important to treat uveitis as soon as it begins. Even if you have treated it before, uveitis can come back again. If you have new or recurring symptoms, make an appointment with your doctor.4