We Should Collaborate With Our Doctors
Growing up, I got it into my head that doctors were akin to authority figures or bosses. What they said was law — and we’d have to obet. After all, they know better right? Well, sort of.
It's important to acknowledge that medical professionals have gone to school for many, many years. They are due respect and that is undeniable. Many doctors and specialists are incredible, compassionate, thorough, and intersectional. Sure, those doctors seem to be rare — but they do exist. It’s important to give credit where it’s due, and I’ve certainly had a few doctors that have made me feel as though I am truly important. Not just a number. Not just a 15-minute time slot to get through.
We know our bodies better than anyone
That said, we know our bodies more intimately than anyone else does. Professionals may be able to see things we do not, and they may know the reasons and the treatments, but we are the ones experiencing the symptoms. We know what it felt like yesterday compared to today.
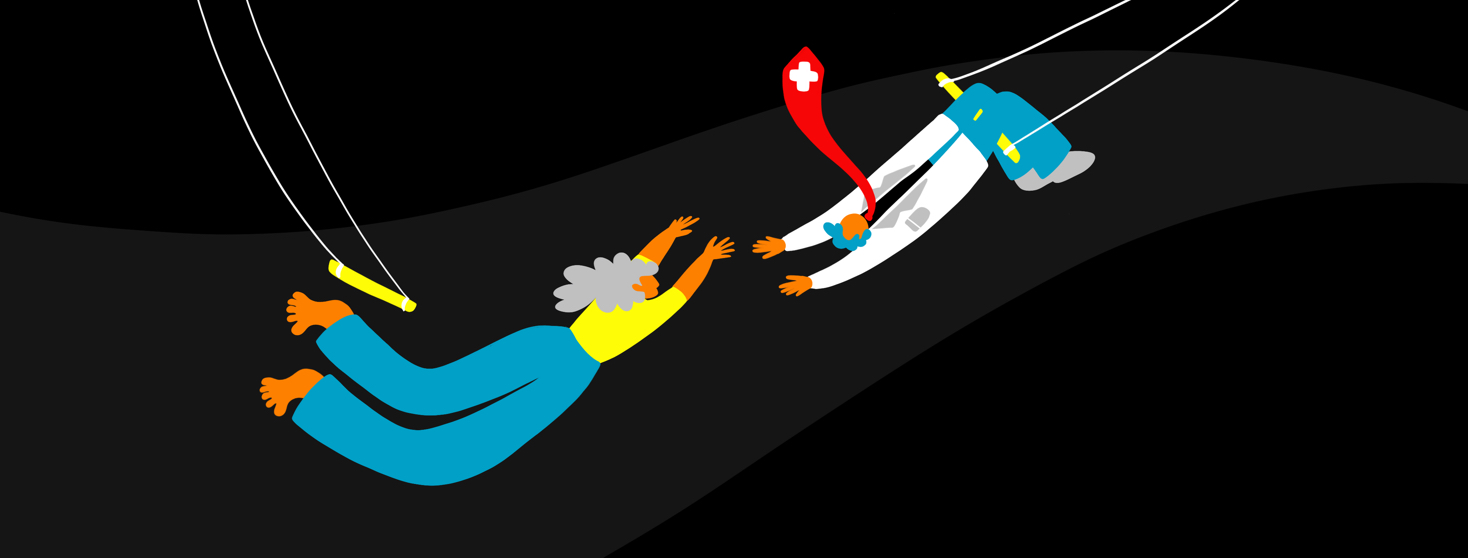
When we see our doctors, it’s important to remember that what happens in the office is a collaboration. Your rheumatologist can’t treat you properly if you’re not honest about your pain or your needs. You still have to be receptive to being treated, and you still have to advocate for your needs.
Many doctors — according to a plethora of people I've spoken to in the chronic illness community — take the position of authority, expecting the patient to fall in line, questioning our need for more answers or our demands for more care. A good doctor will respond to self-advocacy, inquiry, and ideas with respect and care.
The relationship should be respectful and trusting
When it comes to ongoing chronic illnesses marked by vague symptoms and dynamic issues that change day to day or week to week, the relationship between doctor and patient must be respectful and trusting. Because rheumatological diseases are so mysterious, I believe that taking the stance of collaborating with your doctor is vital.
Here are some examples of what collaboration and self-advocacy at the doctor's office that means to me:
- I ask the doctor to explain things to me that I don’t understand, rather than shake my head and pretend that I do for fear of looking stupid.
- I take the doctor's ideas seriously and consider them with an open-mind.
- I tell the doctor what I’m afraid of and what I am not willing to do.
- I ask for education and resources to help me make a decision about medication or something else.
- I request further medical evaluation if I feel that something hasn’t been seen, validated, or proven.
- I provide notes, literature, and anecdotal evidence from my symptom diary, journal, clinical journals, and other trusted sources to my doctor if I need to further a conversation.
- I ask the doctor to make notes of my concerns and to write down any test that they refused to do (and why). I believe it’s important to have these notes in the medical file.
- I am open and honest with my doctor about what is working, and try to start a conversation around how to continue my success.
- I not only ask for standard medical treatments, but I ask about diet, exercise, mental health, social resources, and any other alternative therapies.
- I ask for additional time if needed.
- I ask if virtual and email communication is offered.
- I ask about the doctor's background and perspective
- I ask what the doctor has seen work in other patients with similar issues, ages, mobility levels, etc.
Join the conversation