Stages and Progression
Reviewed by: HU Medical Review Board | Last reviewed: September 2022 | Last updated: November 2025
Axial spondyloarthritis (axSpA) is a type of arthritis that typically starts during the teenage years or young adulthood. Most people start to have symptoms between the ages of 20 and 30. The progression of AxSpA varies widely from person to person. Some people have a fast progression, while others have a mild or slower progression.1
There is no single pattern of progression that applies to everyone with axSpA. But knowing how severe your disease is, how genes affect axSpA, and how progression is measured can help you and your doctor make the best decisions about managing your condition.1,2
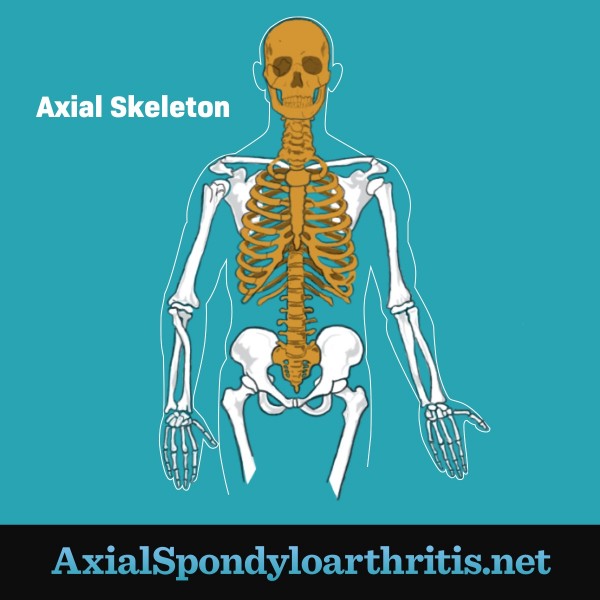
Figure 1. A human axial skeleton
Genes and axial spondyloarthritis
AxSpA has been linked to a variety of genetic risk factors. The presence of the genetic marker HLA-B27 is strongly linked to axSpA. Most people with AS are HLA-B27 positive, compared to less than 10 percent of the general population. However, 1 in 10 people with AS do not have this marker. Other genetic markers also have been linked to axSpA.2
Spectrum of severity
AxSpA may cause a wide range of pain and disability. Experts think of its severity as being on a spectrum. But the condition is usually labeled as 1 of the following:1
- Non-radiographic axSpA (nr-axSpA) – No changes in the sacroiliac joints (the connections of the bottom of the spine to the pelvis) or vertebrae (the bones of the spine) show on an X-ray image. Magnetic resonance imaging (MRI) tests are often needed to detect changes in the SI joints in people with nr-axSpA.
- Radiographic axSpA (r-axSpA, also called ankylosing spondylitis) – Over time, some people with nr-axSpA develop changes in their SI joints that can be seen on X-rays. Ankylosing spondylitis (AS) is diagnosed when X-rays clearly show that the SI joints are affected.
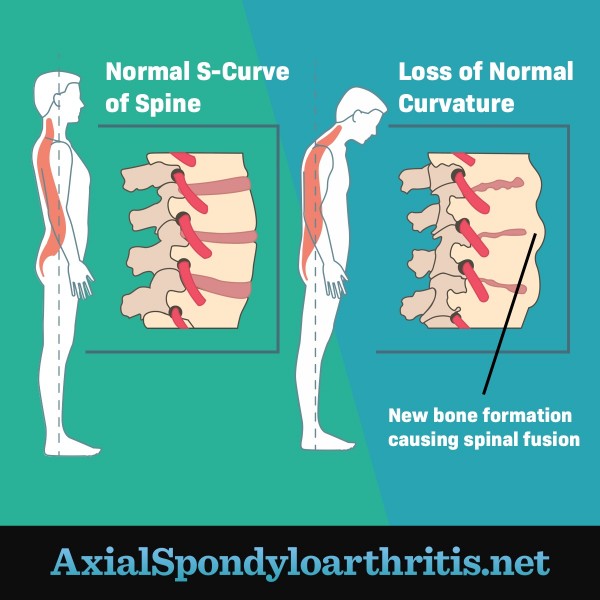
The severe end of the spectrum is bony fusion. This happens when the bones of the spine start to grow together (fuse). This leads to a loss of flexibility and straightening of the spine's normal curvature.1,2
Figure 2. A normal spine compared to a spine that has lost normal curvature
Measuring progression
There is no predictable course of progression for people with axSpA. Doctors do not know why people progress differently.1,2
People with nr-axSpA can progress to radiographic axSpA (AS). When this happens, X-rays that previously showed no joint or bone changes begin to show changes. This progression can take 10 years or more to happen. And not everyone with nr-axSpA will progress to AS.1,2
Another method of measuring progression is looking at inflammatory blood markers. Many people with active inflammatory axSpA have more signs of inflammation in their blood. But not all of them do. Despite their symptoms, many people diagnosed with axSpA do not have these signs of increased inflammation in the blood.1,2
Even if there is never X-ray evidence of disease, those with nr-axSpA can have severe disease and symptoms.1,2
Staging
Some doctors may define ax-SpA as being in an early, progressive, or advanced stage. This is based on your symptoms, X-ray evidence, and whether or not your spine has fused.3,4
Early disease often means no X-ray evidence of disease. Inflammation linked to ax-SpA usually begins before it can be seen in X-ray images. This inflammation leads to symptoms like pain and stiffness.4
Progressive disease describes the slow changes that may or may not eventually show up on X-ray. These changes usually occur over years or even decades. People with progressive axSpA continue to have symptoms, but their X-ray changes remain relatively stable.4
Advanced disease occurs with spinal immobility and bony fusion. This may happen rapidly in some. In others, this may never occur.4
Because the disease progresses differently in different people, there has been a shift over time in how doctors define severity with ax-SpA. Your doctor may or may not talk to you about stages of the disease.3,4
Other things to know
Like many inflammatory conditions, the road traveled by those with axSpA is never a straight course. Many will experience periods of remission, or times when symptoms are milder and easier to manage. There will also likely be flares, or times when symptoms are more active. During a flare, you may experience new symptoms or a worsening of existing symptoms.1,2
No matter the severity, everyone with axSpA should be treated to get their inflammation under control. This will help prevent further damage and preserve spinal function.1,2