Body Pain (Enthesitis)
Reviewed by: HU Medical Review Board | Last reviewed: January 2023 | Last updated: June 2023
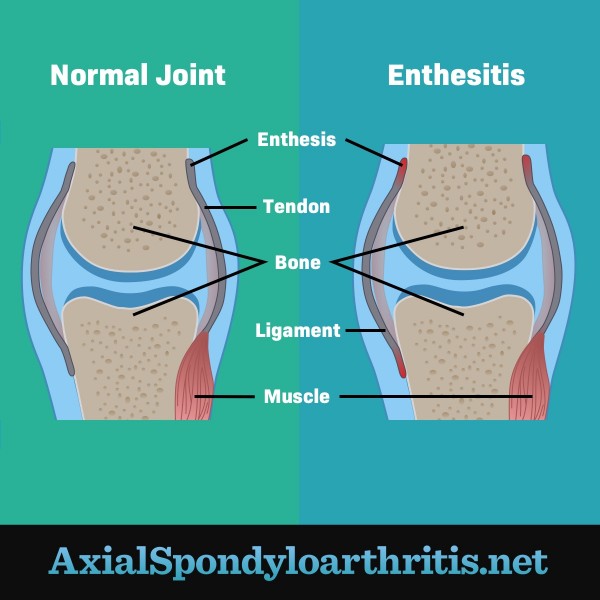
If you have axial spondyloarthritis (axSpA), some parts of your body likely hurt more than others. One of these areas may be where your ligaments or tendons attach to your bone. These areas are called the entheses. Inflammation in these areas is called enthesitis. Enthesitis causes soreness and swelling.1
Figure 1. A joint without inflammation versus an inflamed joint with enthesitis
What causes enthesitis?
Experts do not fully understand the cause of enthesitis. They think it is the result of an overactive immune system. AxSpA is known as an immune-mediated inflammatory condition. This means your immune system attacks healthy tissue by mistake.1
In people with axSpA, the immune system mistakes the entheses for foreign invaders and attacks them. This leads to inflammation, pain, and stiffness.1
What are the symptoms of enthesitis?
Enthesitis is an early and common symptom of axSpA. Multiple areas of the spine (called your axial skeleton) can have enthesitis. This can cause a range of body pain in your neck, back, or hips. Other common areas where enthesitis occurs include:1,2
- Back of the heels (Achilles tendon)
- Arch or sole of the feet (plantar fasciitis)
- Knees
- Tops of the feet
- Fingers and toes
- Elbows
- Shoulders
- Ribs or chest wall
The type of discomfort caused by enthesitis varies from person to person. It can include:1,2
- Pain
- Stiffness
- Tenderness
- Warm to the touch
- Difficulty moving the affected area
In some cases, enthesitis can lead to new bone growth called bone spurs.1
Enthesitis and axSpA progression
AxSpA progresses differently in different people. Some people might have a lot of axSpA symptoms, while others might have only a few. Doctors believe that enthesitis is one of the first signs of the inflammation that occurs with axSpA.2
When these areas become inflamed often, the bone starts to break down. The body rebuilds bone tissue, but sometimes too much bone is formed. This can cause the joint to fuse together or the ligaments to harden. This results in pain, stiffness, and loss of movement.2
How is enthesitis diagnosed?
To diagnose enthesitis, your doctor will ask about your medical history and symptoms. They will also perform a physical exam. Imaging and diagnostic tests might be needed to rule out other conditions. These tests may include:1,2
- X-ray
- Magnetic resonance imaging (MRI)
- Ultrasound
- Blood tests
To check for enthesitis, your doctor might use a scoring system. These focus on measuring tenderness at various places on your body. Some of these exams include:3
- Leeds Enthesitis Index (LEI)
- Spondyloarthritis Research Consortium of Canada (SPARCC) Enthesitis Index
- Maastricht Ankylosing Spondylitis Enthesitis Score (MASES)
- The University of California, San Francisco (UCSF) Index
- Berlin Index
There is not a single standard for which system should be used. Your doctor will tell you more about the exam they are performing.3
How is it treated?
There is no cure for enthesitis or axSpA. But symptoms of axSpA, including enthesitis, can be treated. Combining medicines, exercise, and physical therapy is the standard treatment for axSpA symptoms.1,2
Drugs used to treat axSpA include:1,2,4
- Non-steroidal anti-inflammatory drugs (NSAIDs), which help relieve pain and inflammation
- Biologic drugs, which may help slow or stop the progression of the disease. These drugs block key processes in the inflammatory response.
- Steroids, which are strong anti-inflammatories. When used to treat enthesitis, these drugs may be injected into the joints or areas of pain.
- Disease-modifying antirheumatic drugs (DMARDs), which work to suppress the body’s overactive immune response
If you think you have enthesitis, talk to your doctor. They can help you find the best way to treat your symptoms and prevent further damage.