Axial Spondyloarthritis Pain
Reviewed by: HU Medical Review Board | Last reviewed: January 2023 | Last updated: November 2025
Spondyloarthritis is a condition that affects the joints and the areas where ligaments or tendons attach to bone. Axial spondyloarthritis (axSpA) refers to a family of conditions that mostly affect the spine. These conditions sometimes affect other joints as well. Back pain is the most common symptom of axSpA.1
How does axial spondyloarthritis pain feel?
The back and joint pain linked to axSpA typically comes on slowly and lasts for 3 months or more. The pain gets worse after rest and better with activity. This is the opposite of osteoarthritis, which is different type of arthritis.1,2
Back pain with axSpA also may cause:1,2
- Waking in the middle of the night
- Morning stiffness that lasts longer than 30 minutes
- Possible buttock pain, which can rotate sides
What causes pain with axial spondyloarthritis?
The cause of axSpA symptoms is most often inflammation. Inflammation can lead to stiffness and/or pain in the spine or other joints.1,3
Your immune system's natural reaction when something is wrong is called the inflammatory response. Your cells may be stressed or damaged, or you might have an infection. In response, your body creates inflammation to fight off the threat. This type of inflammation is usually short-term and goes away quickly.4
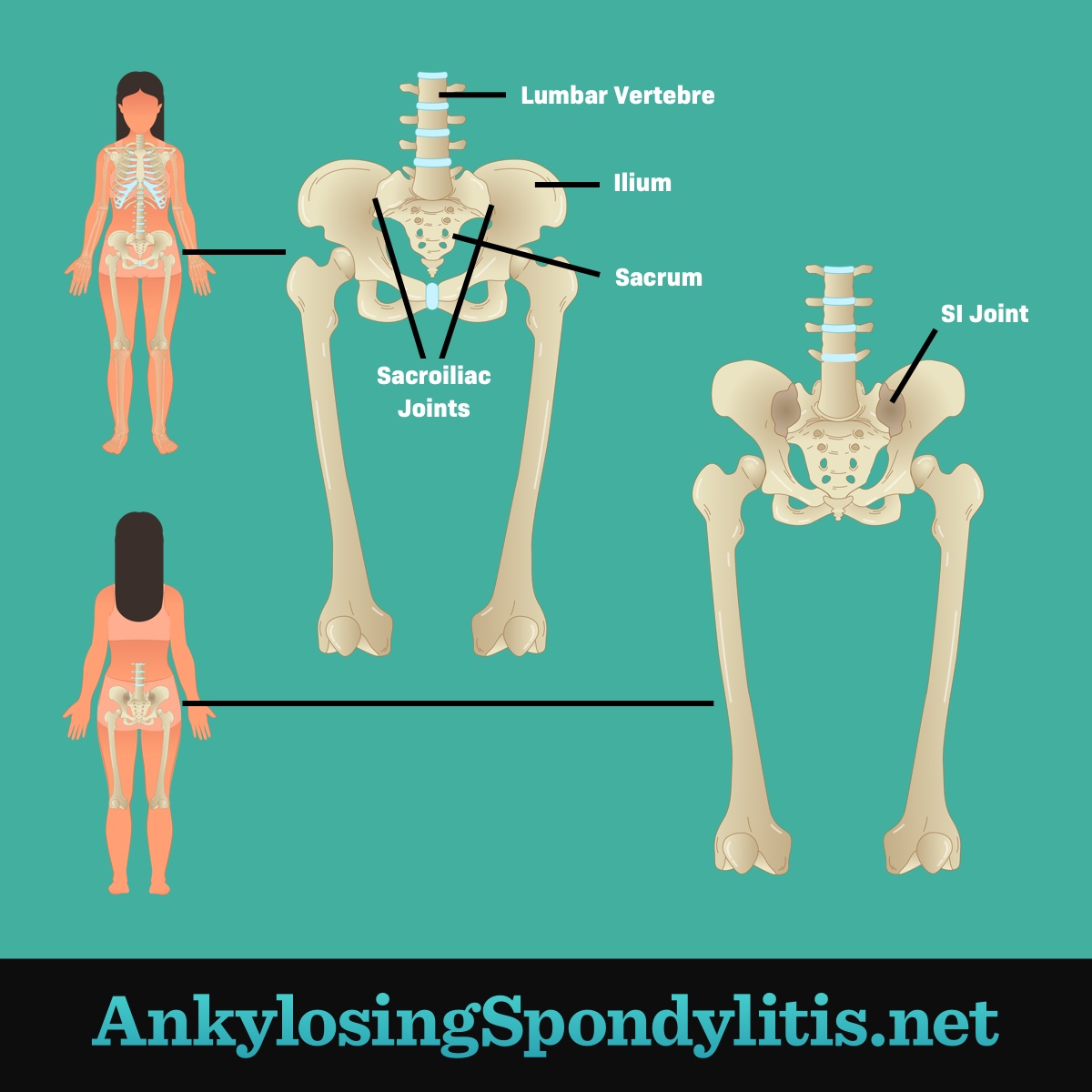
On the other hand, people with axSpA have chronic (long-term) inflammation in their joints. AxSpA mainly affects the joints in the spine and the joints between the base of the spine and the pelvis (sacroiliac joints). But sometimes other joints are also inflamed.5
During an inflammatory response, the cells in your body release chemicals that cause your blood vessels to get bigger. This lets more blood flow to the area, allowing healing cells to respond. The increased blood flow also causes the site to turn red, feel warm, and swell up. Meanwhile, your cells also tell your nerves to send pain messages to your brain.6
The SI joint
Where does the pain occur?
People usually feel axSpA pain in their back. The sacroiliac (SI) joints, which connect the lower spine to the pelvis, are often affected in axSpA. This is known as sacroiliitis. Sacroiliitis may cause pain in the pelvis, hips, or lower back.1,3
In addition to joints, axSpA can affect the places where tendons and ligaments join with bone. Inflammation in these areas is known as enthesitis.2
AxSpA pain can show up in a variety of places outside of the spine. These include the hips, chest, heels, and shoulders.1
Hip pain
Inflammation of the SI joint can feel like hip pain. The hip joint itself may also be affected by axSpA. Sometimes this can lead to pain in the groin or buttocks. Hip pain can cause you to have trouble walking.2
Chest pain
The places where your ribs attach to your breastbone can become inflamed in axSpA. This can lead to chest pain and stiffness of your chest wall. In some advanced cases, the ribs can grow together (fuse) with the spine or chest.7
Chest pain from axSpA can be hard to tell apart from lung or heart problems. If you have any chest pain, seek medical attention right away to rule out an emergency.7
Heel pain
Pain and tenderness in the foot and heel are common in axSpA. Your feet have many tendons and ligaments that can be affected by axSpA.2
The most common area of pain is the heel. This is called Achilles tendonitis. Pain at the bottom of the foot called plantar fasciitis is also a common cause of heel pain. As with hip pain, it can be hard to walk when your feet hurt.2
Shoulder pain
Another common symptom of axSpA is shoulder pain. This can occur when the tendons and bones of your shoulder are inflamed.2
How is pain treated?
Treatment of pain and other symptoms of axSpA usually involves a combination of prescription drugs, physical therapy, and exercise. Drugs used to treat axSpA include:2
- Non-steroidal anti-inflammatory drugs (NSAIDs) – Can help relieve pain and inflammation
- Corticosteroids (steroids) – May be used for short-term relief of inflammation
- Biologic medicines – May help slow or stop the progression of the disease by blocking key processes or compounds involved in the inflammatory response
- Disease-modifying antirheumatic drugs (DMARDs) – May help relieve pain and inflammation, especially in people who cannot take biologic drugs